The following is a guest blog from Alvin H. Danenberg, DDS, a renowned nutritional periodontist and certified LANAP clinician, and author of Crazy-Good Living!: Healthy Gums, Healthy Gut, Healthy Life. The original post can be found on Dr. Danenberg’s website.
Mouth cancer accounts for 2% – 4% of all cancer cases; however, mouth cancer is increasing in frequency. A specific mouth cancer, oral squamous cell carcinoma (OSCC), makes up 90% of all mouth cancers. Unfortunately, the 5-year survival rate for patients with OSCC is 40% -50%. Since there is relatively no pain with OSCC, early detection is critical but rare.
If we knew what was causing mouth cancer, we might be able to nip it in the bud. There is new research suggesting that OSCC might be caused or aggravated by an old enemy – Porphyromonas gingivalis (P. gingivalis).[1]
Porphyromonas gingivalis
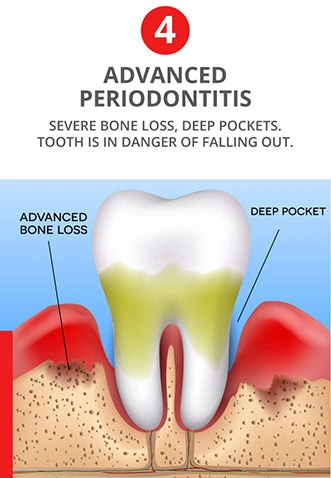
P. gingivalis is a major bug in chronic periodontitis. Its aggressive behavior in dental plaque may be a direct result of chronic systemic inflammation and a compromised host response.[2] Once P. gingivalis becomes pathogenic, the immune system has a difficult time killing it.
Resulting damage to the jawbone from periodontitis is more than a result of bacteria. It is predominantly a result of chronic inflammation created by activation of the immune system to try to kill off P. gingivalis.[3] It is interesting that P. gingivalis can penetrate into epithelial cells and exit from epithelial cells, all along increasing chronic periodontal infection.[4] This bacterium can also penetrate other cells and travel to various parts of the body, leading to other diseases.[5]
Research & OSCC
Research has shown that P. gingivalis will spread to initial lesion sites of OSCC in the soft tissues of the mouth.[6] Another study found that oral cancer cells and cancer stem cells became more aggressive after repeated infection by P. gingivalis.[7] Tumor-like changes appeared to occur with long-term infection from P. gingivalis.
If periodontal disease were diagnosed and treated as soon as possible, then the tendency for P. gingivalis to increase the potential for epithelial cells to become malignant might be halted.
Treatment of Periodontitis
One of the most effective methods to destroy P. gingivalis, which can live inside epithelial cells and in the infected spaces under the gum tissues around teeth, is the LANAP(R) laser protocol. The LANAP protocol also has been shown to stimulate regeneration of damaged jawbone, periodontal ligament, and cementum on the tooth root surface.[8] Here is an animated video that shows how the LANAP laser procedure is performed.[9] This procedure does not require cutting the gum tissues or placing stitches. Patients usually go about their normal routine the next day.
In addition to treating periodontitis, the practitioner should emphasize nutrition and lifestyle changes. It is also important to enhance the immune system and eliminate chronic systemic inflammation. A nutrient-dense, anti-inflammatory diet will go a long way in assisting the body to heal and protect itself going forward.