Laser-Assisted Ridge Preservation
Take full control of extraction and implant cases with the LARiP™ Protocol – available only on the PerioLase® MVP-7™. With the LARiP™ Protocol, you can stabilize, build and regenerate bone in extraction sockets without the use of membranes while delivering extraordinary results

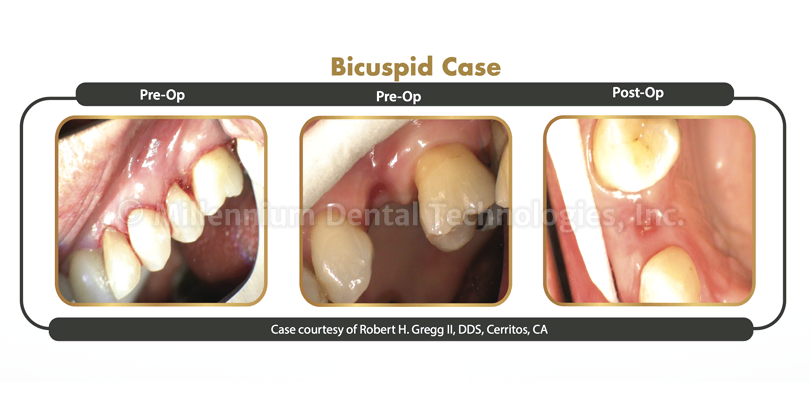
Bicuspid case
Case courtesy of Robert H. Gregg II, DDS, Cerritos, CA
Why the LARiP™ Protocol?
Bone in extraction sockets naturally degrades and recedes, leading to depressions within the ridge and placing the patient at risk for future implant failure.
The LARiP™ Protocol is designed to decrease bone resorption following tooth extraction, preserve the ridge and increase bone graft stability, as well as avoid bony defects.
Laser-assisted ridge preservation has been shown to deliver better clinical outcomes including greater ridge width following tooth extraction compared with traditional debridement with a curette.1
The unique wavelength of the PerioLase® MVP-7™ Nd:YAG laser penetrates up to 6 mm in tissue and bone to eliminate pathogens in extraction sites while leaving healthy connective tissue intact.2,3,4 Meanwhile, the pulse durations of the PerioLase® MVP-7™ provide more conductivity to congeal blood and create a thermogenic clot for bone graft material, eliminating the use of membranes. This helps accelerate healing and reduces the probability of complications.
1. Osman RA, Elkilani NS, Adawy HA, Attia MS. Evalualtion of laser assisted ridge preservation combined with platelet rich fibrin and/or bone. ADJG, 2022; pages 135-143, volume 9, issue 1.
2. Gold SI, Vilardi MA. Pulsed laser beam effects on gingiva. J Clin Periodontol. 1994;21(6):391-6.
3. Harris DM, Yessik M. Therapeutic ration quantifies laserantesepsis: ablation of Porphyromonas gingivalis with dental lasers. Laser Surg Med. 2004;35(3):206-13.
4. JDent Res; March 20, 2014. American Association for Dental Research 43rd Annual Meeting, Charlotte, NJ. 93 (Spec Issue A); Abstract 428.
